At Microsoft’s AI for Good Lab, we’ve been working with partners at the University of Washington, the Fred Hutchinson Cancer Center, and other institutions to explore whether artificial intelligence can help bring greater clarity, accuracy, and trust to breast cancer screening.
This week, our joint research team released the results of a new study published in Radiology, detailing a promising AI approach that aims not just to detect cancer—but to do so in a way that radiologists can trust and patients can understand.
The challenges with current breast cancer screening
Breast cancer is the most common cancer among women worldwide. In the United States alone, one in eight women will be diagnosed with breast cancer in her lifetime. Early detection through screening is the most powerful tool available to save lives, with a 20% to 40% reduction in mortality for women aged 50-69—yet it remains an imperfect science.
Magnetic Resonance Imaging (MRI) is among the most sensitive screening tools available, especially for women at higher risk. But for all its sensitivity, MRI comes with serious trade-offs: high rates of false positives, significantly increased anxiety for patients, and unnecessary biopsies. The problem is especially acute for the nearly 50% of women who have dense breast tissue—a condition that not only increases the risk of breast cancer but also makes it harder to detect abnormalities through traditional imaging methods like mammograms.
Too often, these challenges translate into a troubling equation: more scans, more uncertainty, and more follow-up procedures that turn out to be unnecessary. In fact, only a small fraction—less than 5%—of women undergoing breast MRI screening are ultimately diagnosed with cancer.
A smarter model, built for the real world
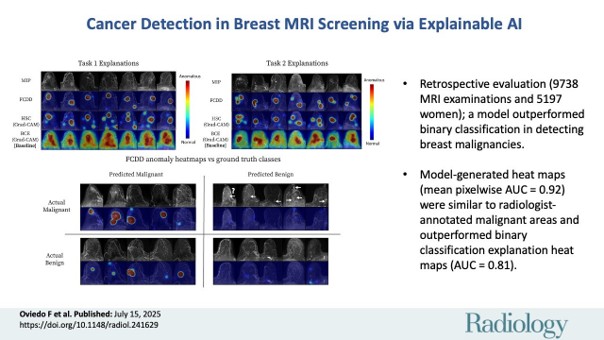
The model—called FCDD (Fully Convolutional Data Description)—is based on anomaly detection rather than standard classification. That’s an important shift. Instead of trying to learn what every possible cancer looks like, the model learns what normal breast scans look like and flags anything that deviates.
This approach is particularly effective in real-world screening settings where cancer is rare and abnormalities are highly varied. Across a dataset of over 9,700 breast MRI exams, the model was tested in both high- and low-prevalence scenarios—including realistic screening populations where just 1.85% of scans contained cancer.
Here’s what we found:
- Improved accuracy in low-prevalence populations: FCDD outperformed traditional AI models in identifying malignancies while dramatically reducing false positives. In screening-like settings, it achieved double the positive predictive value of standard models and cut false alarms by more than 25%.
- Exceptional explainability: Unlike most AI models, FCDD doesn’t just give a “yes” or “no”—it generates heatmaps that visually highlight the suspected tumor location in the two-dimensional MRI projection. These explanation maps matched expert radiologist retrospective annotations with 92% accuracy (pixel-wise AUC), far exceeding other models.
- Generalizability across institutions: Without retraining, the model maintained high performance on a publicly available external dataset and an independent internal dataset, suggesting strong potential for broader clinical adoption.
Making AI impactful, not just impressive
This model is more than a technical achievement. It’s a step toward making AI useful in clinical workflows—providing triage support, reducing time spent on normal cases, and focusing radiologists’ attention where it matters most. By improving specificity at high sensitivity thresholds (95–97%), the model could help reduce unnecessary callbacks and biopsies, easing emotional and financial burdens for patients.
Importantly, the code and methodology have been made open to the research community. You can explore the project here: GitHub Repository, and the paper here.
As with all AI in healthcare, the path to impact requires more than algorithms. It requires trust. Trust is built not only by performance metrics but also by transparency, interpretability, and a clear understanding of the clinical context in which these tools are deployed.
Where we go from here
We still have work ahead. The model will need to be tested prospectively in larger, diverse clinical populations. But the results are promising—and they mark an important shift in how we think about the role of AI in medicine. Rather than asking doctors to trust a black box, we’re building models that shine a light on what they see and why.
“We are very optimistic about the potential of this new AI model, not only for its increased accuracy over other models in identifying cancerous regions but its ability to do so using only minimal image data from each exam. Importantly, this AI tool can be applied to abbreviated contrast-enhanced breast MRI exams as well as full diagnostic protocols, which may also help in shortening both scan times and interpretation times,” said Savannah Partridge, Professor of Radiology at the University of Washington and senior author of the study. “We are excited to take the next steps to assess its utility for enhancing radiologist performance and clinical workflows.”
AI will not replace radiologists. But with the right design and oversight, it can give them sharper tools and clearer signals to increase confidence in evaluating difficult cases.
Breast cancer is a global challenge. With AI, we have a chance to detect it earlier, reduce unnecessary interventions, and ultimately save more lives. That is a future worth building toward—one pixel, one scan, and one breakthrough at a time.